Research program : Respiratory diseases and the environment
Home > Team 3 > Research program > Axe 5
Responders and non-responders to new ex vivo therapies
Magali Taulan-Cadars, Karine Délétang, Jessica Varilh, Solenne Bleuse, Marion Nadaud, Caroline Raynal, Anne Bergougnoux, Arnaud Bourdin, Olivier Cazorla, Fares Gouzi
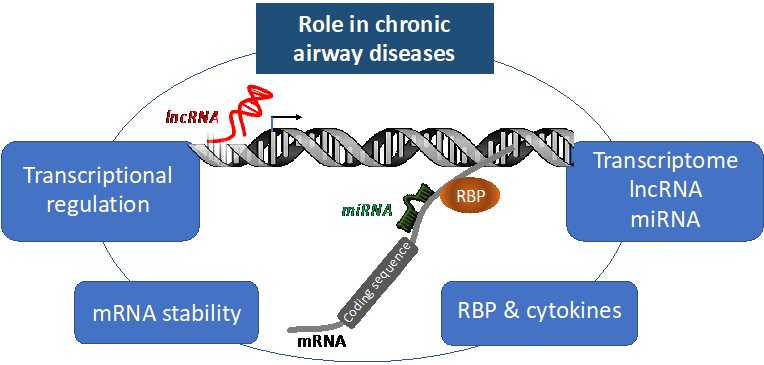
COPD and cystic fibrosis are both chronic diseases of the airways, with distinct etiology, characterized by a decline in lung function resulting from chronic inflammation. Nowadays, the therapies proposed are mainly symptomatic in COPD or remain limited in cystic fibrosis; the search for innovative strategies for the design of new drug molecules remains essential. We propose to research the regulatory elements that participate in the development of chronic diseases characterized by inflammation, to define new molecular circuits associated with these diseases that offer new therapeutic opportunities.
Objective 1: Modulation of CFTR gene expression
We have previously shown that the identification of regulators of CFTR gene expression offers new therapeutic targets (oligonucleotide strategy, international patent PCT/EP2014/069522, SATT-AxLR) in cystic fibrosis1. We are continuing our work in this disease and decided to extend the strategy used to COPD.
Objective 2: Role of anti-inflammatory proteins in cystic fibrosis and COPD
We are also targeting protective proteins against the inflammatory response, including TTP and CCSP2, which are dysregulated in chronic airway diseases. TTP, an RNA-binding protein (RNA-BP or RBP), is a negative post-transcriptional controller of mRNAs encoded by key inflammation genes, including IL2, IL6, IL8, and TNFα, through its binding at their 3’UTR extremity. We are studying its mode of regulation to propose a targeted therapeutic approach for CF and COPD.
Objective 3: Role of non-coding RNAs in cystic fibrosis and COPD
Non-coding RNAs, miRNAs and lncRNAs, which are involved in epithelial homeostasis and the inflammasome in the context of cystic fibrosis and COPD, offer targets for an innovative therapeutic proposal. We recently defined that miR-101 and miR-181, over-expressed in cystic fibrosis and COPD, control the expression of key proteins in the WNT pathway and involved in the inflammatory response, such as the WISP1 protein3. We are also studying the expression profile of miRNAs (miRseq) in order to identify new biomarkers in cystic fibrosis and COPD.
Objective 4: Restoration of the splicing defect
We also applied antisense oligonucleotide strategy (AON) for other CF mutations4 located deep in the introns that affect normal splicing by creating the insertion of an intronic part in the normal RNA sequence5. The efficacy of these AONs for splicing redirection is currently being evaluated in ex-vivo epithelia obtained from patients carrying intronic mutations.
Keywords : Non-coding RNA, RNA-BP, Inflammation, AON strategy, airway epithelium
Fundings