Research program : Respiratory diseases and the environment
Home > Team 3 > Research program > Axe 1
Responders and non-responders in the clinic
Maurice Hayot, Engie Ahmed, Clément Boissin, Sébastien Bommart, Arnaud Bourdin, Jérémy Charriot, François Bughin, Fares Gouzi, Jean Pierre Mallet, Emilie Passerieux, Pascal Pomiès
Therapeutic interventions in a disease as heterogeneous as COPD are based on personalized approaches to improve the functional and vital prognosis and restore a better quality of life for patients. Our proposal is to study the ability to modify the trajectory and nosology of the disease depending on the presence or absence of response to a therapeutic intervention. This approach will lead to distinguishing differential mechanisms according to the type of response, thus opening the way to targeted and effective long-term interventions. For this, our work is oriented towards 3 main types of methods :
Objective 1 : Innovation in global interventions targeting the active behavior of the patient in his environment.
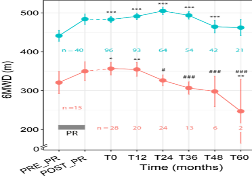
The respiratory rehabilitation offered to COPD patients does not provide the same benefits for all patients benefiting from similar programs. Thanks to the network of collaborations that we have established with respiratory rehabilitation establishments and structures at regional, national and international level, we are developing specific expertise aimed at determining the functional and cellular biomarkers characteristic of the trajectories of responders/non-responders to rehabilitation. The original work we are carrying out aims to develop the concept of “rehabilitation throughout life” by relying on hybrid approaches bringing together human intervention, connected objects, telemedicine and telerehabilitation. The long-term objective is to target the clinical and biological criteria predicting responses to rehabilitation in order to propose dedicated interventions likely to reinforce favorable trajectories and influence others in order to improve the quality of life and the evolutionary prognosis of the disease, as soon as possible, or even before it occurs.
Objective 2 : Specific intervention techniques acting on the structures of the respiratory system and its interactions with other systems.
- Bronchial thermoplasty and endoscopic lung volume reduction (ELVR) are targeted interventions for eligible patients based on a multi-scale assessment. Quantification of changes in emphysematous lesions and spatiotemporal distribution of lesions likely predict ELVR, while impaired mucociliary clearance may indicate benefits of bronchial thermoplasty or tailored interventions. In this area, we are conducting several PHRC-type clinical trials.
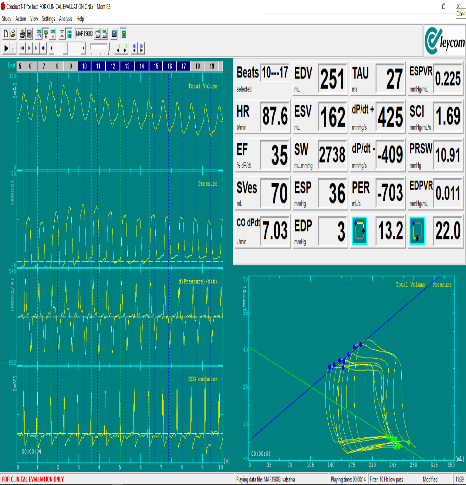
- Dysfunction of the right ventricle, but also potentially of the left ventricle, can be a predictor of the benefits of ELVR for which we are developing a translational model. Elastase-induced emphysema in rats with LPS-induced exacerbation is now well established in our laboratory. The observation of a specific group of COPD patients with abdominal aortic aneurysm is an epidemiological observation that our experimental model seems to confirm, facilitating in the future the study of specific mechanisms in humans.

Objective 3 : Molecular and pharmacological intervention targeting chronic airway inflammation.
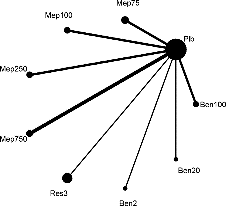
Th2-type airway inflammation is likely to be targeted by the use of monoclonal antibodies directed against IL5, IL4, IL13, IL33 and its receptor ST2, TSLP and others, currently under development in asthma and COPD and in patients with features of Asthma and COPD Overlap. Glucocorticoids are another insufficiently explored axis in case of exacerbation. Current associated biomarkers such as blood or sputum eosinophil count, or exhaled NO concentrations, suffer from several weaknesses that merit the identification of more stable and predictive biomarkers. Our team will develop the analysis of responders in clinics with the aim not only to identify molecular and functional biomarkers but also to determine resistance mechanisms in non-responder patients in order to find new therapeutic solutions.
Keywords : Rehabilitation, telerehabilitation, telemedicine, T2 inflammation, biomarkers, bronchial thermoplasty, endoscopic lung volume reduction, airway epithelium
